Dieser Beitrag ist auch verfügbar auf:
![]() Deutsch
Deutsch ![]() Italiano
Italiano
e?????^'?v?????Jئ?V??????C????+????
Inspired by an article from Focus, we have written a brief summary here of current research in the field of brain stimulation with direct current.
At one moment, it illuminates our rooms; in the next, it provides the unfathomable network of electrical impulses that control our bodies. While most of us limit ourselves to the simple act of flipping a light switch, scientists delve deep into the mysteries of the electrical signals that permeate our biological system. With groundbreaking advances in neurology, researchers are attempting to decode and modulate these electrical signals to find therapeutic solutions for diseases such as Parkinson’s, stroke, and depression.
The idea that electrical impulses are shot directly into our brains through tiny openings in the skull may send shivers down the spine. However, this invasive procedure, known as deep brain stimulation, has the potential to change lives. It’s not just scientific curiosity but an established therapeutic technique that has already helped thousands of Parkinson’s patients worldwide. For those suffering from severe motor disorders, the implantation of a brain pacemaker means a rebirth of a life where everyday tasks become possible again.
However, the scope of deep brain stimulation extends beyond motor disorders. Recent discoveries have shown that this technique also has the potential to influence emotions. Medical professionals are working to expand its application spectrum and test the method for various mental illnesses. Particularly impressive are the initial successes in treating severe depressive disorders.
Psychiatrist Thomas Schläpfer from the University of Bonn and neurosurgeon Volker Coenen from the University of Freiburg seem to have found a promising neural target for their electrodes. Through targeted stimulation of a fiber bundle connected to the brain’s reward system, they were able to make significant progress in treating patients with severe depression.
Research in this field is not yet complete. While some teams are investigating the benefits of deep brain stimulation for addiction disorders, post-traumatic stress disorders, and dementia, others are using electrotherapy techniques to help stroke patients regain lost abilities. For example, scalp direct current stimulation has shown success in improving speech abilities after a stroke.
The journey into the world of electrical neuromodulation is fascinating and complex at the same time. While we follow the wonderful stories of patients who have benefited from these treatments, we must not overlook the ethical questions that arise from them.

N???W????jS^??&?ۥjب?)Ğ?r)?5뫢Z ?ƥE?(???
From 2008 to 2010, a patient observation study was conducted by the physiotherapy department of Städtisches Krankenhaus Kiel. The aim was to determine the extent to which microcurrent therapy has an impact on Parkinson’s and multiple sclerosis patients.
The patient observation was conducted by the head physiotherapist Inge Metag.
W????jT??k?jب?+nw(?xZ?ȧ???h?'?????
Between August 2008 and April 2010, 99 patients diagnosed with conditions such as Parkinson’s, multiple sclerosis, amyotrophic lateral sclerosis, and restless legs syndrome were specifically treated with the CLINIC-master/VITAL-master. The choice of this treatment was based on good results for similar complaints and the flexible program variety of the devices. All 99 patients were able to forego conventional electrotherapy and instead utilize Clinic/Vital-master therapy, which could be individually tailored to their respective symptoms. The study concludes that the treatment led to an unprecedented improvement in the quality of life and daily well-being of long-term patients.
1?a??%?
The study included 99 patients with various neurological conditions (77 with Parkinson’s, 12 with MS, 2 with ALS, and 8 with restless legs syndrome). The average age was 67.3 years. One-third of the patients were employed, and 50% could manage their daily lives without assistance. Patients had prior experience with various forms of physical therapy before undergoing treatment with the Clinic-master/Vital-master. There was no clear structure in medical care, and patients had different preferences for active or passive therapy approaches.
34 patients were in stationary geriatric clinic care, 22 in day clinic geriatric care, and 21 in outpatient physical therapy treatment. The Clinic-master/Vital-master therapy was applied over a period of 12 weeks without prior active or passive individual measures. Doctors had no objections to the new method but did not pose direct content-related questions.
The study demonstrates that Clinic-master/Vital-master therapy could be well integrated into the existing spectrum of therapies and served as an effective treatment for the observed conditions. Patients and doctors were receptive to the new approach, despite the absence of detailed questions about the method.
N???g?? i???
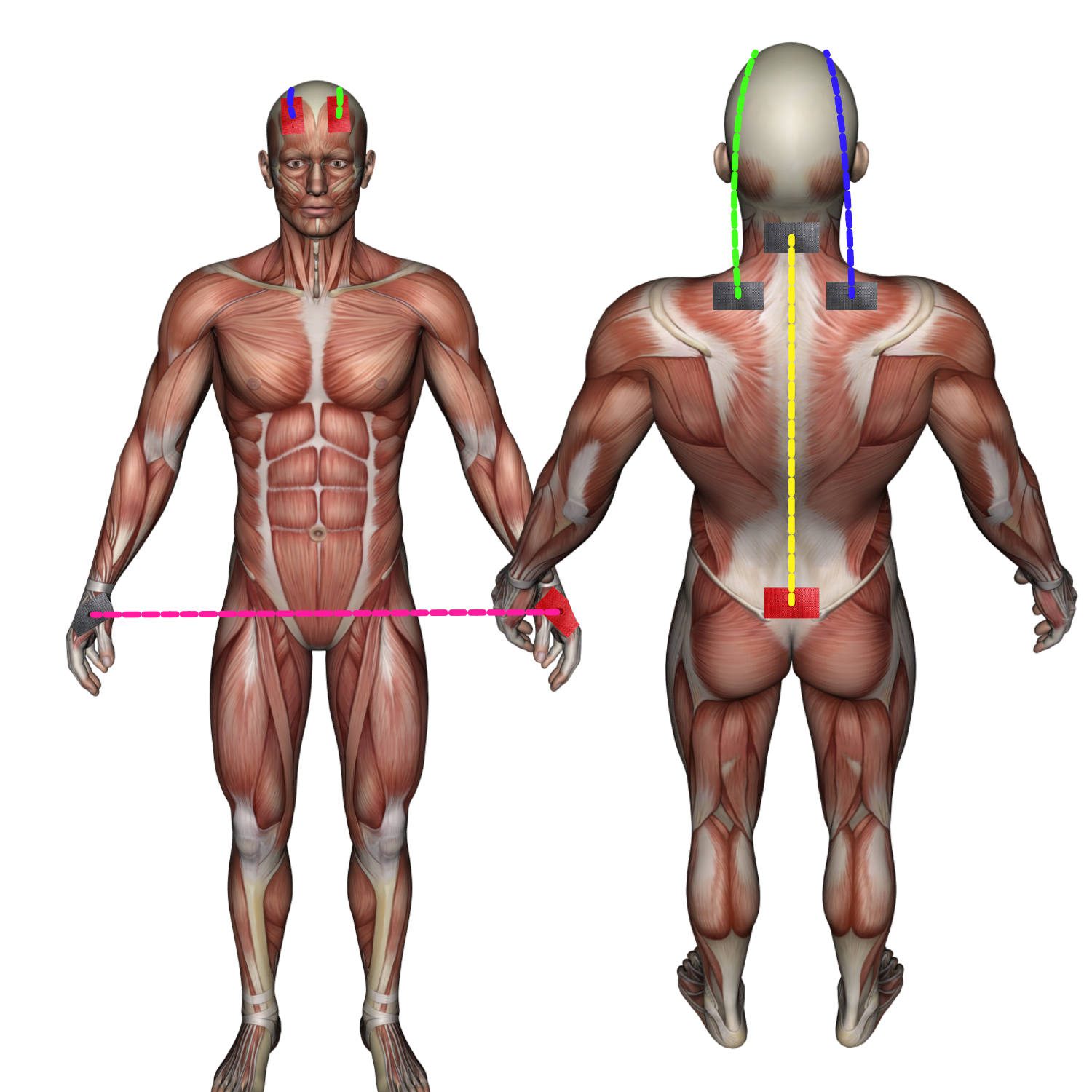
In the study on the treatment of Parkinson’s, MS, and ALS patients, there was a deliberate avoidance of strict adherence to a single therapy program or a specific electrode arrangement. This considered the variable symptoms and intensities of these conditions. Treatment was adjusted daily to the individual situation of the patients, made possible by the variety of available programs. For inpatients, daily application was planned for two weeks (a total of 10 applications). Outpatient patients received 10 applications, distributed over two sessions per week for a period of five weeks. Flexibility and individualization of the therapy approach were emphasized.
E?.??(|I^r??q?R?)???b?w????)?}7??jw@-
The clinical study showed significant treatment successes in patients with long-standing chronic conditions such as Parkinson’s, MS, and ALS that could not be achieved with traditional therapy methods. The customization of electrotherapy programs played a crucial role.
For Parkinson’s patients, the “Regeneration" program was effective in reducing rigidity, while the “Neuralgia" program effectively attenuated intention and resting tremors. Standing and gait instability were also reduced. For patients who could not clearly articulate their symptoms, the “Autonomic Compensation" program served as a good treatment starting point.
The choice of programs was flexible and based on the current symptoms as well as discussions between the practitioner and the patient. Additionally, programs could also be effectively used for non-neurological issues such as arthritis or rheumatism.
The surprisingly positive overall results included:
- Improved flexibility of movement
- Reduction or disappearance of tremors
- Enhanced stability in standing and walking
- Improved wheelchair mobility
- Increased life satisfaction and more active participation in family and social life.
The study suggests that individually adaptable electrotherapy can achieve significant improvements in the treatment of these patient groups.